Unless your condition is causing significant problems or is rapidly getting worse, treatment for lumbar disc herniation usually begins with non surgical treatment. Most people with a herniated lumbar disc get better without surgery. As a result, it is usually recommended that patients try non operative treatments for at least six weeks before considering surgery.
At first, your Physiotherapist at Physio Med may want your low back immobilized. Keeping the back still for a short time can calm inflammation and pain. This might include a period of bed rest. Lying on your back can take pressure off sore discs and nerves. However, our Physiotherapists usually advise against strict bed rest and prefer their patients to do ordinary activities using pain to gauge how much is too much. In rare cases in which bed rest is prescribed, it is usually used for a maximum of two days.
A back support belt is sometimes used for patients with lumbar disc herniation. The belt can help lower pressure inside the problem disc. Our patients are encouraged to gradually discontinue wearing the support belt over a period of two to four days. Otherwise, their trunk muscles begin to rely on the belt and start to weaken and atrophy (shrink).
Our Physiotherapy treatments focus on relieving pain, improving back movement, and fostering healthy posture. The first goal of our treatment is to control symptoms. Your Physiotherapist will help you find positions and movements that ease pain. Treatments of heat, cold, ultrasound, and electrical stimulation may be used in the first few sessions. Lumbar traction may also be used at first to ease symptoms of lumbar disc herniation. In addition, our Physiotherapist may use hands-on treatments such as massage or spinal manipulation. These forms of treatment are mainly used to help reduce pain and inflammation so you can resume normal activity as soon as possible.
Your physiotherapist will show you how to keep your spine safe during routine activities. You'll learn about healthy posture and how posture relates to the future health of your spine. We will teach you about body mechanics, how the body moves and functions during activity. Our physiotherapists teach safe body mechanics to help you protect the low back as you go about your day. This includes the use of safe positions and movements while lifting and carrying, standing and walking, and performing work duties.
The next part of our program will include a series of strengthening exercises for the abdominal and low back muscles. Working these core muscles helps our patients begin moving easier and lessens the chances of future pain and problems. Aerobic exercises such as walking or swimming are used for easing pain and improving endurance.
We will work closely with your doctor and employer to help you get back on the job as quickly as reasonably possible. You may be required to do lighter duties at first, but as soon as you are able, you'll begin doing your normal work activities. Our Physiotherapists can do a work assessment to make sure you'll be safe to do your job. We may suggest changes that could help you work safely, with less chance of re-injuring your back.
A primary purpose of your Physiotherapy is to help you learn how to take care of your symptoms yourself and prevent future problems. We'll provide you with a home program of exercises to continue improving flexibility, posture, endurance, and low back and abdominal strength. Our Physiotherapist will also discuss strategies you can use if your symptoms flare up.
When patients simply aren't getting better during their therapy program, or if the problem is becoming more severe, surgery may be suggested.
Post-surgical Rehabilitation
Rehabilitation after surgery is more complex. Some patients leave the hospital shortly after surgery. However, some surgeries require patients to stay in the hospital for a few days.
During recovery from surgery, patients should follow their surgeon's instructions about wearing a back brace or support belt, and should be cautious about overdoing activities in the first few weeks after surgery.
Although recovery time varies for each patient, as a guideline you may expect to see our Physiotherapists for one to three months, depending on the type of surgery. At first, your Physiotherapists may use treatments such as heat or ice, electrical stimulation, massage, and ultrasound to help calm pain and muscle spasm. We provide reassurance to help you deal with fear and apprehension about pain. Then our Physiotherapists will teach you how to move safely while putting the least strain on your healing back. Exercises are used to improve flexibility, strength, and endurance.
When your recovery is well under way, your regular visits to Physio Med will end. Although we will continue to be a resource, you will be in charge of doing your exercises as part of an ongoing home program.
Portions of this document copyright MMG, LLC.
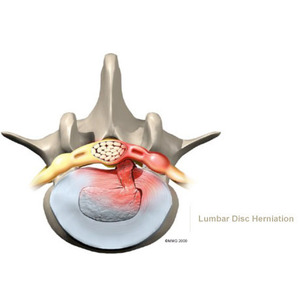





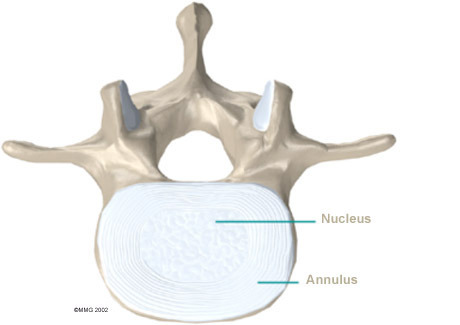
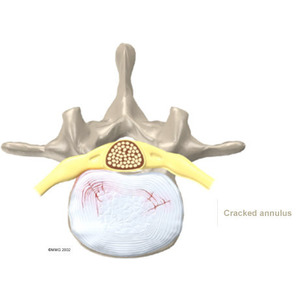
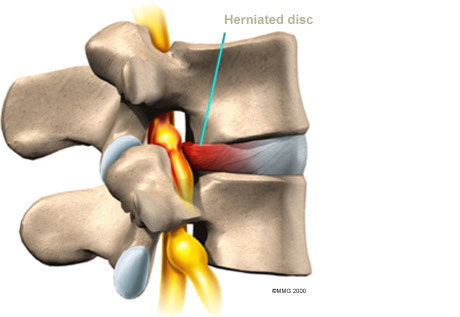 Herniation causes pain from a variety of sources. It can cause mechanical pain. This is pain that comes from the parts of the spine that move during activity, such as the discs and ligaments. Pain from inflammation occurs when the nucleus squeezes through the annulus. The nucleus normally does not come in contact with the body's blood supply. However, a tear in the annulus puts the nucleus at risk for contacting this blood supply. When the nucleus herniates into the torn annulus, the nucleus and blood supply meet, causing a reaction of the chemicals inside the nucleus. This produces inflammation and pain. A disc herniation may also put pressure against a spinal nerve. Pressure on an irritated or damaged nerve can produce pain that radiates along the nerve. This is called neurogenic pain.
Herniation causes pain from a variety of sources. It can cause mechanical pain. This is pain that comes from the parts of the spine that move during activity, such as the discs and ligaments. Pain from inflammation occurs when the nucleus squeezes through the annulus. The nucleus normally does not come in contact with the body's blood supply. However, a tear in the annulus puts the nucleus at risk for contacting this blood supply. When the nucleus herniates into the torn annulus, the nucleus and blood supply meet, causing a reaction of the chemicals inside the nucleus. This produces inflammation and pain. A disc herniation may also put pressure against a spinal nerve. Pressure on an irritated or damaged nerve can produce pain that radiates along the nerve. This is called neurogenic pain.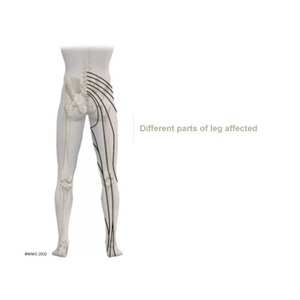
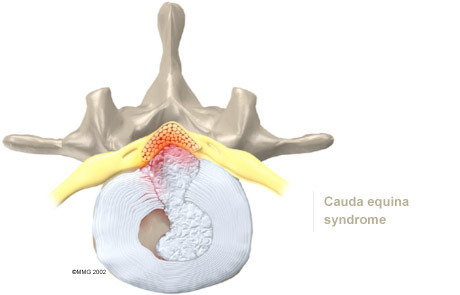
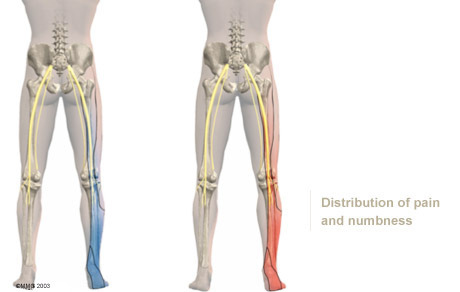 bowel and bladder function. A large disc herniation that pushes straight back into the spinal canal can put pressure on the nerves that go to the bowels and bladder. The pressure may cause low back pain, pain running down the back of both legs, and numbness or tingling between the legs in the area you would contact if you were seated on a saddle. The pressure on the nerves can cause a loss of control in the bowels or bladder. This is an emergency. If the pressure isn't relieved, it can lead to permanent paralysis of the bowels and bladder. This condition is called cauda equina syndrome. Doctors recommend immediate surgery to remove pressure from the nerves.
bowel and bladder function. A large disc herniation that pushes straight back into the spinal canal can put pressure on the nerves that go to the bowels and bladder. The pressure may cause low back pain, pain running down the back of both legs, and numbness or tingling between the legs in the area you would contact if you were seated on a saddle. The pressure on the nerves can cause a loss of control in the bowels or bladder. This is an emergency. If the pressure isn't relieved, it can lead to permanent paralysis of the bowels and bladder. This condition is called cauda equina syndrome. Doctors recommend immediate surgery to remove pressure from the nerves.