When you begin physiotherapy at Physio Med, the rehabilitation program that our physiotherapist prescribes will depend on the specific type of problem (tendonitis or tendinopathy / tendonosis / tendon rupture) present.
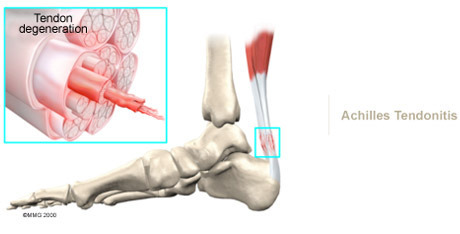
Tendonitis/Tendinopathy
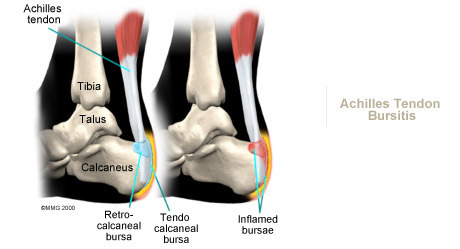
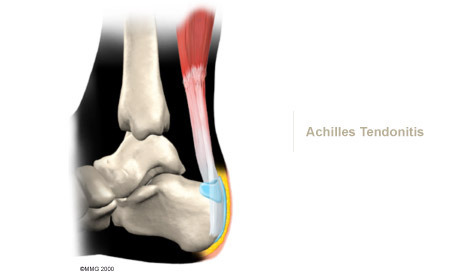
In the past, nonsurgical treatment for tendocalcaneal bursitis and Achilles tendonitis started with a combination of rest, ice, and anti-inflammatory medications prescribed by your doctor.
Since it is now recognized that many tendon problems occur without inflammation, the use of anti-inflammatories and ice have come into question. In the case of true inflammation, the overuse of these modalities may prevent a normal, healing inflammatory process. Preventing inflammation needed to clean up cellular debris in the injured area may lead to delayed or incomplete healing. The result may be future chronic problems of tendonosis and/or tendinopathy.
Many experts suggest that when there is any doubt about inflammation, treatment should proceed as if there are no inflammatory cells present. Our approach would then focus on pain relief and restoring proper motion and weight-bearing so you can return to your usual activities.
If there is an inflammatory process, then the condition should respond fairly quickly to drug and anti-inflammatory interventions. Limiting, but not eliminating, inflammation is the new goal.
Our physiotherapists know when and how to apply cold modalities to reduce swelling and pain, while still allowing the healing inflammatory process. We may also apply treatments such as ultrasound, moist heat, and massage are used to control pain and inflammation. As pain eases, we will progresses your treatment to include stretching and strengthening exercises.
Tendonosis
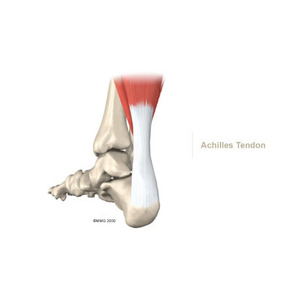
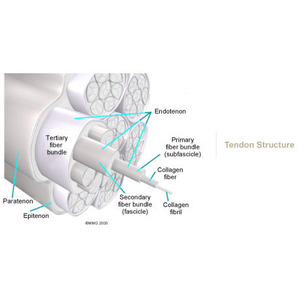
If the problem is one of tendon tissue degeneration, healing and recovery may take longer. This type of injury will not respond to treatment designed to reduce inflammation. Correct treatment of tendonosis involves fostering new collagen tissue growth and improving the strength of the tendon. Rehabilitation following rupture of the tendon is quite different and is described later.
An acute injury needs rest. We recommend that initially, you limit activities that require walking on the sore leg. Although the time required for rehabilitation varies among patients, in cases of Achilles tendinopathy, or when a partial tendon tear is being treated without surgery, patients may require two to three months of physiotherapy.
Your physiotherapist may recommend that a small (one-quarter inch) heel lift be placed in your shoe to minimize stress by putting slack in the calf muscle and Achilles tendon. A similar sized lift will also be placed in the other shoe to keep everything aligned.
Injured tendons shorten and need to be stretched. Only gentle stretches of the calf muscles and Achilles tendon are used at first. As the tendon heals and pain eases, more aggressive stretches are given. Our therapist may also use ultrasound and massage to help the tendon heal.
As your condition improves, exercises to strengthen the calf muscles begin. Strengthening starts gradually using isometrics, exercises that work the muscles but protect the healing area. Eventually, specialized strengthening exercises, called eccentrics, are used, working the calf muscle while it lengthens.
The physiotherapy provided by Physio Med enables patients to gradually return to normal activities. We have specialized programs to guide athletes in rehabilitation that is specific to their type of sport.
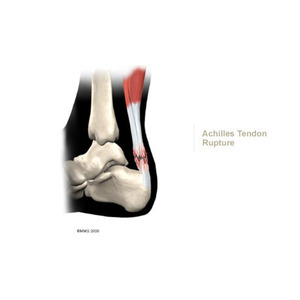
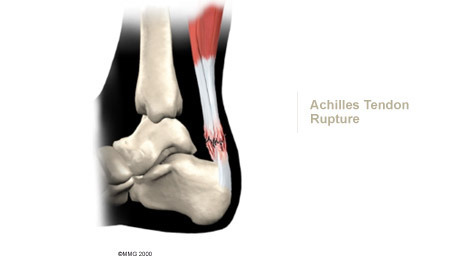
Tendon Rupture
Nonsurgical treatment for an Achilles tendon rupture can take two forms. It is clear that treatment with a cast will allow the vast majority of tendon ruptures to heal, however, many ruptures of the Achilles tendon will need to be surgically repaired.
Nonsurgical treatment might be considered for the aging adult who has an inactive lifestyle. This allows the patient to heal while avoiding the potential complications of surgery. The patient's foot and ankle are placed in a cast for approximately eight weeks. Casting the leg with the foot pointing downward brings the torn ends of the Achilles tendon together and holds them until scar tissue joins the damaged ends. During this time, your physiotherapist will instruct you in safe and proper crutch utilization. After your cast is removed, our physiotherapist may advise the use of a walking boot to limit the stress through the tendon.
Surgery
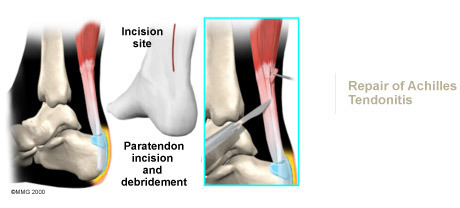
Surgical treatment for Achilles tendonitis is not usually necessary for most patients. Surgery options range from a tenotomy (a simple release of the tendon) to a more involved, open approach of repair.
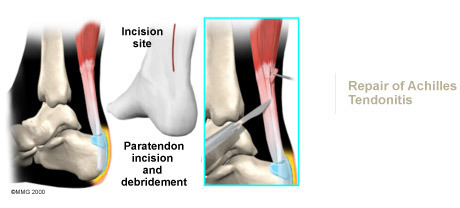
In some cases of persistent tendonitis and tendonosis a procedure called debridement of the Achilles tendon may be suggested to help treat the problem.
This procedure is usually done through an incision on the back of the ankle near the Achilles tendon. The tendon is identified, and any inflamed paratenon tissue (the covering of the tendon) is removed. The tendon is then split, and the degenerative portion of the tendon is removed. The split tendon is then repaired and allowed to heal. It is unclear why, but removing the degenerative portion of the tendon seems to stimulate repair of the tendon to a more normal state.
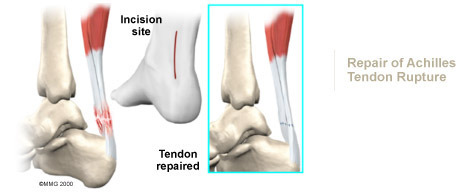
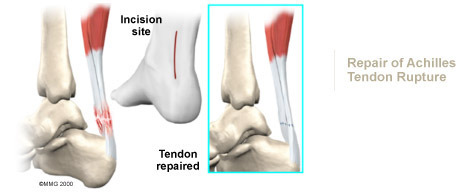
Surgery may also be suggested if you have a ruptured Achilles tendon. Reattaching the two ends of the tendon repairs the torn Achilles tendon. This procedure is usually done through an incision on the back of the ankle near the Achilles tendon. Numerous procedures have been developed to repair the tendon, but most involve sewing the two ends of the tendon together in some fashion. Some repair techniques have been developed to minimize the size of the incision.
In the past, the complications of surgical repair of the Achilles tendon made surgeons think twice before suggesting surgery. The complications arose because the skin where the incision must be made is thin and has a poor blood supply. This can lead to an increase in the chance of the wound not healing and infection setting in. Now that this is better recognized, the complication rate is lower and surgery is recommended more often.
Post-surgical Rehabilitation
Although the time required for recovery is different for each individual, patients are typically placed in a cast, brace or splint for six to eight weeks after surgery to protect the repair and the skin incision. Your physiotherapist will help you learn to properly use crutches to keep from putting weight onto your foot too soon after surgery.
Devices used to immobilize the leg can cause joint stiffness, muscle wasting (atrophy), and blood clots. To avoid these problems, our therapist will have you start doing motion exercises very soon after surgery. Patients typically wear a splint or brace that can easily be removed to do the exercises throughout the day.
In this early-motion approach, you begin our physiotherapy program within the first few days after surgery. Your physiotherapist in Leeds may initially use ice and massage to limit (but not completely prevent) swelling and pain. Massage and ultrasound help heal and strengthen the tendon.
Our physiotherapy treatments eventually progress to include more advanced mobility and strengthening exercises, some of which may be done in a pool. The buoyancy of the water helps people walk and exercise safely without putting too much tension on the healing tendon. The splint is worn while walking usually for six to eight weeks after surgery.
As your symptoms ease and your strength improves, our physiotherapist will guide you through advancing stages of exercise. Athletes often begin running, cutting, and jumping drills by the fourth month after surgery, and although recovery time is different for each patient, they are usually able to get back to their sport by six full months after surgery.
Our goal is to help you keep your pain and swelling under control, improve your range of motion and strength, and ensure you regain a normal walking pattern. When your recovery is well under way, regular visits to the Physio Med will end. Although we will continue to be a resource, you will be in charge of doing your exercises as part of an ongoing home program.
Portions of this document copyright MMG, LLC.